- Solutions
We are here to Help
Medical Billing Companies
Practice Staffing Management
Medical Billing Consultancy
Workforce Extension
Networks & IT support
- Specialities
- Company
- Learn

Transforming Your Healthcare Revenue Cycle
Proactive Denial Management and Accounts Receivable Solutions for Maximum Efficiency
Proactive Denial Management and Accounts Receivable Solutions for Maximum Efficiency
Get a free quote today!


















Free Billing Audit
Comprehensive Account Receivable & Denial Management
We deeply understand the unique financial challenges faced by healthcare providers who experience long receivables cycles that not only delay critical revenue and disrupt cash flow but also place a heavy burden on billing teams and create challenges in financial management. These issues are intensified by both accurate and inaccurate claims denials, creating a complex landscape in financial operations. Pro Medical Billing Solutions offers a healthy solution to these challenges with our specialized Accounts Receivable and Claim Denial Management Services. Our team employs a systematic, detail-oriented approach, ensuring precise and timely reimbursement of claims.
Effective A/R management is crucial, especially for physicians, ambulatory surgery centers, and hospitals, in addressing unpaid or pending claims quickly and efficiently. Our strategic, analytical approach to A/R management is designed to produce significant, measurable, and accurate financial returns, this is not only streamlining your Revenue Cycle but also significantly improves administrative efficiency.
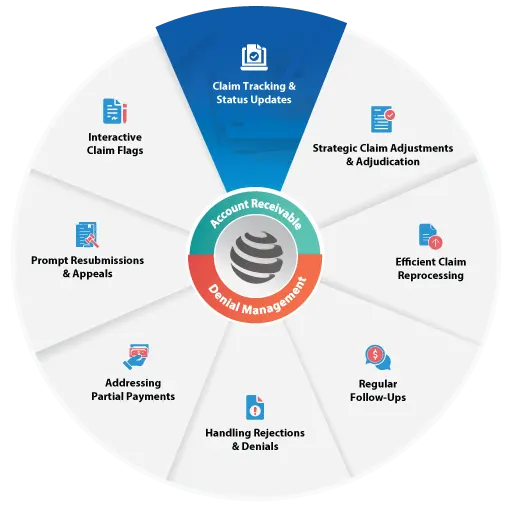
Our A/R & Denial Management Approach
We understand that effective Accounts Receivable (A/R) and Denial Management are more than just financial processes – they’re the lifeblood of your healthcare practice’s financial health. That’s why we’ve crafted an approach that combines empathy, expertise, and efficiency, turning financial challenges into opportunities for growth and stability.
Claim tracking and status updates involve monitoring the progress and current status of insurance claims submitted by healthcare providers. This process includes keeping track of the claim’s journey from submission to payment, and providing regular updates to healthcare providers regarding any developments, such as claim acceptance, denial, or payment processing. Pro Medical Billing Solutions diligently track each claim, regularly updating payment statuses after comprehensive verification through calls and online checks. This ensures you’re always in the loop with the latest claim developments.
Strategic claim adjustments and adjudication refer to the deliberate and planned process of reviewing, modifying, and making decisions on insurance claims with a specific goal in mind. This could involve analyzing claims data to identify patterns, trends, or opportunities for improvement, as well as making informed decisions to optimize claim reimbursement, minimize denials, and ensure compliance with payer policies and regulations.Our team conducts in-depth investigations, adjusting denied or partially paid claims for a balanced financial ledger.
Efficient claim reprocessing involves the swift and effective handling of insurance claims that require reevaluation or resubmission. This process aims to rectify any errors or issues that led to claim denials or underpayments, ensuring that the claims are processed accurately and promptly to expedite reimbursement for healthcare services provided. Pro Medical Billing Solutions tackle resubmissions and appeals head-on, providing additional documentation when needed to secure full payments.
Regular follow-ups on claims entail consistent monitoring and communication regarding the status and progress of insurance claims. This involves reaching out to insurance companies or payers at predetermined intervals to inquire about the status of pending claims, identify any delays or issues, and ensure timely resolution to expedite claim processing and reimbursement.Every 30 days, we conduct follow-ups, providing insights into the status of each claim – whether paid, pending, or denied.
Handling rejections and denials involves managing instances where insurance claims are not accepted or approved by the payer. This process includes investigating the reasons for rejection or denial, correcting any errors or deficiencies in the claim, and resubmitting the claim with necessary adjustments or additional documentation to appeal the decision and secure reimbursement for the healthcare services provided. We quickly address issues like incorrect information or invalid codes, identifying non-payment causes, and reprocessing claims with supplementary details to overturn denials.
Addressing partial payments involves managing situations where insurance companies or payers only partially reimburse healthcare providers for the services rendered. This process includes identifying the reasons for the partial payment, such as coding errors or coverage limitations, and taking appropriate steps to rectify the situation. This may involve appealing the payment decision, providing additional documentation or clarification, or negotiating with the payer to ensure full reimbursement for the services provided. Pro Medical Billing Solutions delves into reasons behind incomplete payments, pursuing reprocessing or appeals with added information to secure the remaining balance.
Prompt resubmissions and appeals involve quickly re-submitting insurance claims or appealing decisions made by payers regarding claim denials, partial payments, or other issues. This process aims to address discrepancies, errors, or misunderstandings in the initial claim submission or payment decision. By promptly resubmitting claims with necessary corrections or providing additional information to support the claim, healthcare providers seek to secure proper reimbursement for the services rendered. Similarly, appealing decisions through formal channels allows providers to challenge unfavorable outcomes and advocate for fair and accurate reimbursement.Our team quickly refiles claims needing extra details, such as X-rays or W9 forms, and crafts detailed appeals with necessary clinical documentation for reconsideration.
Interactive claim flags are indicators or markers within a claims processing system that serve to highlight specific issues, discrepancies, or actions required for a particular claim. These flags are interactive in that they prompt users to take specific actions or provide additional information to address the flagged issues. They help streamline the claims processing workflow by drawing attention to critical areas that may require further review, correction, or follow-up, ultimately improving efficiency and accuracy in claim adjudication.
Why Focus on Denials Management? How We Make a Difference
Denials can be frustrating roadblocks in the Revenue Cycle, but at Pro Medical Billing Solutions, we see them as opportunities for improvement. It’s our team of experts, with their deep understanding of healthcare finance, who make the real difference. They bring the insight, compassion, and dedication that technology alone cannot provide. This proactive analysis helps us identify trends, improve billing practices, and reduce future denials, turning each challenge into a learning opportunity. We believe that at the core of effective A/R and Denial Management is empathy. Our team is trained to handle each account with the understanding that we’re not just dealing with numbers but with people’s health and well-being. This human-centered approach ensures that we remain respectful, compliant, and sensitive to the nuances of healthcare billing.
We don’t just manage your A/R and denials; we’re committed to strengthening the financial backbone of your practice. Our approach is designed to give you peace of mind and the freedom to focus on providing excellent healthcare, knowing your finances are in expert hands.
Looking for an expert service?
If you are looking for expert and cost-effective Medical Billing services, Get in touch with us today
Let's Connect

Effective Strategies for Reducing Denials in Healthcare Billing
Every healthcare practice is unique, and so are its challenges. Our approach is not one-size-fits-all. We work closely with you to understand the specific nuances of your practice, crafting personalized strategies to reduce denials. By identifying common denial trends and addressing the root causes, we turn potential losses into robust revenue gains.
We believe that at the core of effective billing management lies a deep understanding of human experiences. Every claim tells a patient’s story, and every denial represents a chapter that needs careful attention. Our team, equipped with expertise and empathy, dives into these stories. Our mission is to empower your practice by transforming the way you handle Medical Billing, turning complexities into streamlined success.
The first step in our denial management process is to identify the reasons for the denial. To achieve this, we use advanced software systems that are designed to analyze every claim and identify any that have been denied. This helps us quickly identify any issues that need to be addressed and enables us to take action to resolve them promptly.
Once we have identified the denied claims, we categorize them according to the reason for the denial. We have a wide range of categories that we use to classify the denials, such as missing information, incorrect coding, and non-covered services. This allows us to analyze the data and identify any patterns or trends that may indicate underlying issues that need to be addressed.
Once we have identified the reason for the denial, we take appropriate action to resolve the issue and resubmit the claim. This may involve correcting errors in the billing data or providing additional information that was missing from the initial claim. Our team works diligently to ensure that the resubmitted claim is accurate and complete, increasing the chances of it being accepted by the payer.
We understand the importance of tracking the progress of each resubmitted claim. Our team closely monitors the status of each claim, tracking it through the entire process until it is accepted and paid by the payer. This allows us to quickly identify any issues that may arise and take corrective action promptly, minimizing payment delays.
In addition to resolving denied claims, we also have a prevention mechanism in place to reduce the likelihood of future denials. We regularly review our billing data and identify any patterns or trends that may indicate issues that need to be addressed. By proactively addressing these issues, we can prevent future denials and help our clients maximize their revenue.
Finally, we continually monitor future claims to ensure that they are accurate and complete before they are submitted. Our team works closely with our clients to ensure that they are aware of any issues or errors that may arise and help them address these issues promptly to prevent denials.
What Makes Pro Medical Billing Solutions Special?
As a well-known Medical Billing Service provider, we take pride in our track record of consistently delivering accurate and timely results, ultimately enhancing revenue for our respected clients. We use state-of-the-art expertise to streamline the Medical Billing process, decrease errors, and improve productivity, all while providing exceptional customer service.
Pro Medical Billing Solutions has a team of incredibly talented and deeply experienced Medical Billing and Coding specialists. Our expertise isn’t just about handling billing requests. It’s a passionate commitment to ensuring your financial success in the Revenue Cycle Management industry.
Why Do Healthcare Professionals Choose Our Medical Billing Services?
Rapid Revenue Recovery
0
Days
First-Pass Resolution
0
%
Denial & Rejection
0
% - 10%
Short Turnaround Time
0
Hours
Electronic Claim
0
%
Electronic Payment
0
%
Client Retention
0
%
Revenue Increase
0
%
Let's Connect
Rapid Revenue Recovery
0
Days
First-Pass Resolution
0
%
Denial & Rejection
0
% - 10%
Short Turnaround Time
0
Hours
Electronic Claim
0
%
Electronic Payment
0
%
Client Retention
0
%
Revenue Increase
0
%
We're here to help
We're available 24/7 - Schedule a call with one of our experts now.
Here are the top specialties, we are helping healthcare physicians throughout the United States to address their Medical Billing & Credentialing challenges.
Our team of experts specializes in the following areas, which are known to be the most impactful for improving Medical Billing efficiency and accuracy.
If you are searching for a reliable Medical Billing Company – You’ve found it – Contact us today to learn more about our services!
If you are searching for a reliable Medical Billing Company – You’ve found it –
Contact Us
today to learn more about our services!
Our Expertise
- Patient Scheduling & Registration
- Verification of Benefits
- Authorization & Referral
- Medical Billing
- Medical Coding
- Medical Billing Financial Audit
- Charge Entry & Payment Posting
- Billing & Coding Audit
- Denial Management
- AR Management
- Revenue Cycle Optimization
- Old AR Recovery
- Patient Billing & Statements
- Collections Services
- Patient Help 24/7
Here are the top specialties, We are helping healthcare physicians throughout the United States to address their Medical Billing & Credentialing challenges.
Our team of experts specializes in the following areas,which are known to be the most impactful for improving Medical Billing efficiency and accuracy.
If you are searching for a reliable Medical Billing Company -You’ve found it – contact us
today to learn more about our services!
Our Expertise
- Patient Scheduling & Registration
- Verification of Benefits
- Authorization & Referral
- Medical Billing
- Medical Coding
- Medical Billing Financial Audit
- Charge Entry & Payment Posting
- Billing & Coding Audit
- Denial Management
- AR Management
- Revenue Cycle Optimization
- Old AR Recovery
- Patient Billing & Statements
- Collections Services
- Patient Help 24/7
Medical Billing Software We Leverage for Revenue Cycle Management
Here are some Industry top listed EHR being operated by us.




















Our Esteemed Clients' Testimonials
For the past 15 months, Pro Medical Billing Solutions has consistently delivered incredible collection results, with first-pass rates surpassing industry standards. Their high responsiveness and effective Revenue Cycle Management services make them the go-to choose for any practice looking to take control of their billing.

Dr. Mukherjee Ranadev | CO-FOUNDER
Digestive Associates (Nevada)
We rely on Pro MBS for our medical billing operations and analysis. Our collaboration with Pro MBS has allowed us to excel over the last five years. We had a few patients’ inflows initially, and we ended up getting many more clients, Pro MBS helped us scale.

Dr. Charles Sisson | MD
Integrated Medical Consultants (Colorado)
Thanks to Pro Medical Billing Solutions, our practice has seen a significant improvement in our billing and collection processes. Their team is always up-to-date with the latest industry changes, and they have provided excellent support to our staff. We would highly recommend their services to any healthcare provider.

Jennifer Hartley | Administrator
Adams Physical Therapy Services, Inc. (Indiana)
We have been using Pro Medical Billing Solutions for several months, and we have been extremely satisfied with their services. They have helped us to optimize our billing and coding practices, resulting in improved cash flow for our practice. We highly recommend them to other healthcare providers.

Marissa Vazquez | Office Manager
Presence Therapy (Nevada)
Pro MBS has provided excellent satisfaction for our Medical Billing and Coding operations. We conduct regular meetings with their team. They are updated with current industry trends and keep very high standards for quality service. We consider them as an extension of our business office.

Huiping Xu | MD
Whole Health Professional PLLC (Texas)
Pro Medical billing Solutions has numerous strengths. One of many is effective communication, which kept me aware of billing updates and claim processes. I am impressed with the swift claim processing and the turnaround time for claims. appreciate Pro Medical Billing Solutions for providing constant support.

Sandra Diaz | CEO
South Main Clinic (Texas)
We are pleased with Pro Medical Billing Solutions' billing and coding services and highly endorse them to anyone looking for a proficient billing company. Collaborating with Pro Medical Billing Solutions has been effortless, and we are deeply grateful for their services.

Jennifer G. Walker D | DC
Colorado Chiropractic Center (Colorado)
As the CEO of Big Dog Pharma, I would highly recommend Pro Medical Billing Solutions for your Medical Billing and Coding processes. Over the past four years of collaboration, I have found them responsive, prompt, and helpful. Through our extension, we reduced our staff requirements and significantly improved our revenue stream.

Johnny Gilbert | CEO
Bird Dog Pharma (Texas)
I look back over the past five years of our relationship, and I can predict what the coming five years would look like. I can see immense growth opportunities for both of our organizations with the partnership that we have been able to develop. I absolutely recommend Pro Medical Billing Solutions.

Dr. Michael Farrel | DC
Spine Correction Center (Colorado)
Frequently Asked Questions
Account Receivable and Denial Management Services are specialized financial services tailored for healthcare providers. They focus on efficiently managing and collecting payments due from insurance companies and patients. Denial Management, a critical component of these services, involves identifying, investigating, and appealing unpaid or underpaid claims due to denials by payers.
The goal is to optimize revenue cycle performance, reduce the time between service delivery and payment, and minimize the financial impact of claim denials.
To minimize claim denials, we implement a multi-faceted approach:
Pre-Claim Audits: We conduct thorough audits before claims submission to ensure accuracy in patient information, coding, and billing.
Payer Policy Updates: Our team stays informed on the latest payer policies to prevent denials due to outdated or incorrect information.
Training and Education: Regular training sessions for our staff and clients on the latest coding standards and healthcare regulations.
Data Analytics: Utilizing advanced analytics to identify denial patterns and areas prone to errors, allowing us to proactively address issues.
When a claim is denied, our process involves:
Immediate Review: Quickly reviewing and analyzing the reason for denial.
Corrective Action: Rectifying any errors or providing additional information required.
Appeal Process: If necessary, we initiate an appeal, presenting a well-documented case to overturn the denial.
Feedback Loop: Learnings from denials are fed back into our process to prevent similar issues in the future.
Yes, we offer comprehensive analytics and reporting services. These include:
Denial Trend Analysis: Reports on common reasons for denials and recommendations for prevention.
Performance Metrics: Regular updates on key performance indicators such as claim settlement times, denial rates, and recovery amounts.
Custom Reports: Tailored reports based on the specific needs of your practice, providing insights into areas like payer behavior, patient demographics, and service line profitability.
We provide robust customer support, including:
Dedicated Account Managers: Each client is assigned an account manager for personalized service.
Help Desk Support: Access to our help desk for immediate assistance with billing and software issues.
Regular Updates and Consultations: Scheduled meetings to discuss performance, address concerns, and provide industry updates.
Protecting patient information is paramount. We adhere to stringent security protocols, including:
HIPAA Compliance: Strict adherence to HIPAA guidelines to ensure patient data privacy and security.
Data Encryption: Utilizing advanced encryption techniques for data storage and transmission.
Regular Audits: Conducting periodic security audits and updating our protocols to address any emerging threats.
Patient demographics are a foundational element of the healthcare billing process, and errors or inaccuracies in this information can have a significant impact on denial management. Ensuring that patient demographic data is complete and up-to-date is essential for minimizing claim denials and optimizing the Revenue Cycle.
To maximize revenue with improved claims denials management, healthcare providers should implement effective strategies and best practices as mention below
By following these steps and continuously monitoring and adapting denial management processes, healthcare providers can minimize revenue loss due to denials and maximize their overall revenue.
- Analyze historical denial data to identify common patterns, such as specific payers, denial reasons, or coding errors.
- Ensure accurate and timely claims submission.
- Implement Revenue Cycle Management (RCM) software and denial management tools to automate claim tracking and identify issues promptly.
- Establish a structured workflow for managing denials.
- Develop a robust denial appeal process. Craft customized appeals that address specific denial reasons and include supporting documentation, such as medical records and coding references.
- Conduct root cause analysis to identify the underlying reasons for recurring denials.
- Ensure that medical records and clinical documentation support the services billed.
Denial Management is an integral part of a successful Revenue Cycle Management strategy that helps healthcare organizations achieve financial sustainability and provide quality patient care. Denial Management aims to ensure that healthcare providers receive appropriate reimbursement for the services they deliver, minimize financial disruptions caused by denials, and maintain compliance with regulatory and contractual obligations.
Let's Outsource Medical Billing Services To Us
-
Quick Turnaround Times
-
Monthly Coding Audit
-
Timely AR Follow-Up
-
Revenue Cycle Optimization
-
24/7 Helpdesk Support
-
Expert Medical Billers
-
Advance Cash Flow
-
Reasonable Pricing
-
Qualified Coding Auditors
-
Real-Time Insurance Verification
-
Auditing Complex Denials
-
Unlimited Physician Credentialing
-
30 Days Free Trial
-
Denial Management
-
Healthcare Analytics
-
Medical Billing Consultation
0
+
Years of Experience
0
+
Providers
0
+
Software
0
+
Specialities
0
+
Years of Experience
0
+
Providers
0
+
Software
0
+
Specialities
Thousands of providers growing their practice with PROMBS.
"Now It's Your Turn"!


























Pro Medical Billing Solutions is doing an incredible job of boosting our revenue and improving our cash flow. They are excellent at communicating with the insurance providers and are prompt in addressing issues. We're immensely grateful for their wonderful efforts, and we give a thumbs-up to their entire team.